Pulmonary Hypertension: In-Depth Guide to Symptoms, Diagnosis, and Treatment
Pulmonary Hypertension: A Detailed Overview
Understanding Pulmonary Hypertension
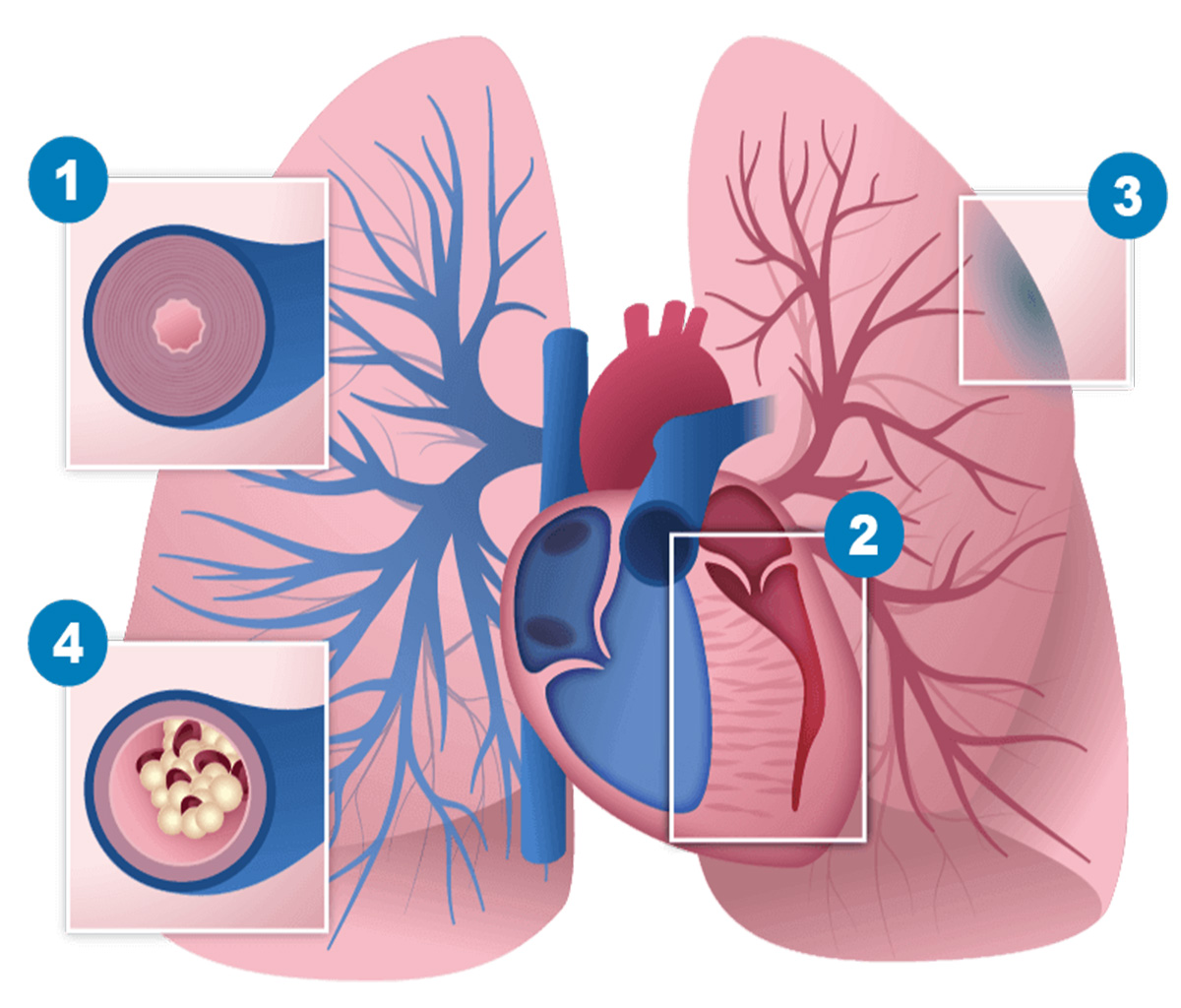
Pulmonary Hypertension (PH) is a serious and chronic condition characterized by abnormally high blood pressure in the arteries of the lungs. This increased pressure places extra strain on the heart, potentially leading to heart failure if not properly managed. PH is often associated with other underlying health conditions, highlighting the importance of early diagnosis and proactive management to improve patient outcomes.
Types of Pulmonary Hypertension
PH is classified into five distinct categories based on its underlying causes:
1. Pulmonary Arterial Hypertension (PAH)
- Caused by narrowing, thickening, or stiffening of the arteries in the lungs, leading to increased pressure.
- Includes idiopathic PAH, heritable PAH, and PAH associated with connective tissue diseases, HIV, and congenital heart defects.
2. PH Due to Left Heart Disease
- The most common form of PH, resulting from conditions that affect the left side of the heart (e.g., valve disease, left ventricular dysfunction).
- Causes pressure to back up into the lungs.
3. PH Due to Lung Diseases or Hypoxia
- Associated with conditions like COPD, interstitial lung disease, sleep apnea, and high-altitude exposure.
- Long-term low oxygen levels contribute to damage in the lung vessels.
4. Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
- Caused by undissolved blood clots in the lung arteries, leading to persistent blockages.
- Notably, this type of PH is potentially curable with surgical intervention.
5. PH with Unclear Multifactorial Mechanisms
- Encompasses hematologic, systemic, and metabolic disorders with complex and not fully understood causes.
Symptoms of Pulmonary Hypertension
Symptoms of PH can vary in severity and may include:
- Shortness of breath (initially during activity, eventually even at rest)
- Fatigue (persistent tiredness and low energy)
- Chest pain or pressure (often confused with angina)
- Palpitations (irregular or rapid heartbeat)
- Swelling (edema in ankles, legs, and abdomen)
- Cyanosis (bluish tint to lips and skin)
- Dizziness or fainting (syncope)
Causes and Risk Factors
PH can develop due to various factors, including:
- Genetic predisposition (inherited mutations)
- Chronic lung diseases (such as COPD, pulmonary fibrosis, and sleep apnea)
- Heart conditions (affecting the left side of the heart)
- Blood clots (chronic clots in the lungs, as seen in CTEPH)
- Connective tissue diseases (like scleroderma and lupus)
- Other risk factors (including obesity, chronic liver disease, HIV, drug use, and chemical exposure)
Diagnosis of Pulmonary Hypertension
Diagnosing PH typically involves:
- Medical history and physical examination
- Echocardiogram (ultrasound of the heart)
- Right heart catheterization (measures pressure in lung arteries)
- Pulmonary function tests (to assess lung function)
- CT scan or MRI (to visualize lungs and arteries)
- Blood tests (to identify underlying conditions)
- 6-minute walk test (to evaluate functional status)
Treatment Options for Pulmonary Hypertension
Treatment for PH aims to manage symptoms, improve quality of life, and slow disease progression. Options include:
- Medications (such as vasodilators, anticoagulants, diuretics, and oxygen therapy)
- Surgical interventions (including atrial septostomy, pulmonary thromboendarterectomy (PTE), and lung or heart-lung transplant)
- Lifestyle changes (such as increased physical activity, dietary adjustments, smoking cessation, and managing comorbidities)
Prognosis and Living with Pulmonary Hypertension
The prognosis for PH varies depending on its cause, severity, and response to treatment. With early diagnosis and proper care, many patients can lead fulfilling lives. Continuous monitoring and treatment adjustments are essential for managing this condition effectively.





